Company settles Ohio Medicaid allegation suit
Published 12:00 am Saturday, June 19, 2021
Centene agrees to pay Ohio $88M
COLUMBUS (AP) — Centene Corp. has agreed to pay Ohio $88.3 million to settle a lawsuit alleging the pharmacy benefit manager overbilled the state’s Medicaid department for pharmacy services it provided, the state’s top lawyer announced Monday.
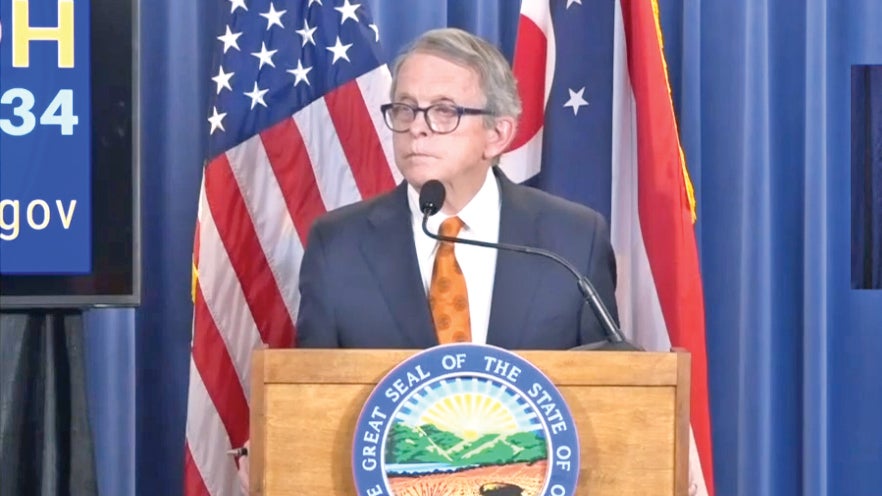
Republican Attorney General Dave Yost said the settlement is the first and largest in the nation secured by a state attorney general against a pharmacy benefit manager. PBMs are third-party companies that manage health care plans, including Medicaid, which serves 2.9 million Ohioans.
Yost’s suit alleged Centene and its subsidiary, Buckeye Health Plan, conspired to misrepresent the costs of pharmacy services it provided Ohio, which included the prices of prescription drugs.
The attorney general said state investigators uncovered a sophisticated scheme to bill unearned dollars known only at the top levels of health care companies. Yost alleges a series of contract breaches, including double-billing, failing to disclose drug discounts that affected prescription costs and artificially inflating fees.
Yost said that Centene’s Buckeye Health Plan used two sister companies, Envolve Health Solutions and Health Net Pharmacy Solutions, to administer pharmacy benefits, which raised initial questions. Under the settlement agreement, St. Louis-based Centene does not admit fault.
In a statement, the company said it respects “the deep and critically important relationships we have with our state partners” and the agreements “reflect the significance we place on addressing their concerns and our ongoing commitment to making the delivery of healthcare local, simple and transparent.”
“Importantly, putting these issues behind us allows us to continue our relentless focus on delivering high-quality outcomes to our members,” said Brent Layton, company president of health plans, markets and products.
Talks continue with a plaintiffs’ group “in an effort to bring final resolution to these concerns in other affected states,” the company said.